RESEARCH
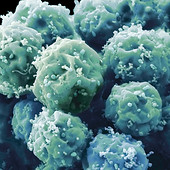
Our translational research program is based upon the rationale that the eradication of malignant stem cells is essential for achieving long-term remission and that extrinsic factors from the microenvironment, including the immune system, play a key role in the pathogenesis, progression and therapeutic response in cancer.
STEM CELLS
Stem cells have the unique property to generate stem cells (self-renewal) and all the other cells with specialized functions (differentiation) in a specific tissue.
Cancer stem cells (CSC) share the same cellular and molecular mechanisms that regulate healthy stem cells but lack the control systems that maintain homeostasis and prevent uncontrolled proliferation.
Given that CSCs have the capacity of regenerating cancer, they are responsible for driving disease progression and relapse.

MICROENVIRONMENT
The microenvironment (ME) also called 'niche' is defined by the cells, molecules and structures (including blood vessels) that surround and support other cells and tissues.
CSCs generate and activate their own tumor microenvironment (TME), by recruiting surrounding cells to work for CSCs' own benefit. The dynamic interaction of CSCs with the TME is essential to stimulate cancer regeneration, propagation, and therapy-resistance, thereby promoting disease progression and relapse.

THERAPEUTICS
The detection and eradication of CSCs remain critical for developing curative treatments for patients.
The interactions of CSCs with the TME actively contribute to oncogenesis and therapy-resistance, while suppressing healthy tissue homeostasis.
Therefore,
a greater understanding of the interplay between CSCs, proliferating tumor cells and niche is needed for the development of new and more effective therapeutic strategies in cancer.
Acute leukemia is the most common cancer in children, but can occur at any age. The outlook for most acute leukemias tends to be better in children than in adolescents or adults.
Acute leukemias can grow quickly, so they need to be treated as soon as they are found. These aggressive blood cancers can cause tiredness, weakness, pale skin, bleeding or bruising, fever, weight loss, bone and joint pain, and other symptoms.
Types of acute leukemia

ACUTE LYMPHOBLASTIC LEUKEMIA (ALL)
Most common in children, characterized by overproduction of immature dysfunctional lymphocytes (lymphoblasts or leukemic blasts). Different types:
-
Pre-B ALL – blasts resembling immature B-cell features;
-
B-cell ALL (B-ALL) – blasts displaying mature B-cell surface markers;
-
T-cell ALL (T-ALL) – blasts characterized by T-cell development markers.

ACUTE
MYELOID LEUKEMIA (AML)
Mostly associated with old age, characterized by an overproduction of immature and dysfunctional myeloid cells (myeloblasts or leukemic blasts).
Name given to a group of acute leukemias associated with different types of myeloid cells (red blood cells, platelets, white blood cells excluding lymphocytes).

ACUTE LEUKEMIA OF AMBIGUOUS LINEAGE (ALAL)
Rare subset (<5%) of acute leukemia associated with a markedly adverse clinical outcome.
Encompasses leukemias which fail to show commitment to either the myeloid, B-, or T-lymphoid lineages (ie, acute undifferentiated leukemia - AUL), or show evidence of commitment to more than one lineage (ie, mixed-phenotype acute leukemias - MPAL).
What is the prognosis?
High-dose (induction) chemotherapy followed by low-dose maintenance therapy for 2-3 years remains the mainstay treatment for acute leukemia.
Therapeutic regimen is adapted to the subtype of leukemia, but precision medicine strategies remain limited.
Despite significant improvement over the last 30 years,
the overall 5-year survival of patients is only ~65%.
Origin of relapse in acute leukemia
In acute leukemia, we refer to cell populations capable of propagating the disease and giving rise to relapse as leukemia stem cells (LSCs). Given their inherent capacity of tumor regeneration, LSCs are responsible for driving disease progression and relapse.
Furthermore, we have experimentally demonstrated that numerous signals from the microenvironment support LSCs, thereby actively promoting leukemia progression and relapse.
Despite these recent discoveries, the mechanisms of therapy-resistance in acute leukemia remain poorly defined, particularly in T-ALL.
OUR RESEARCH STRATEGY
Using bulk and single cell multi-omic (e.g., transcriptomic, genomic, proteomic) approaches, whilst taking advantage of in vivo tools that enable to study LSCs at any stage during leukemia development, our research team aims to understand how LSCs escape immune surveillance and current therapies, and how tumor cells interact with their microenvironment to drive relapse in acute leukemia.
We have successfully established a translational pipeline that incorporates cell-marking strategies and patient-derived xenograft (PDX) models of acute leukemia for pre-clinical testing of novel antileukemic therapies.
Using this translational pipeline, our ultimate goal is to develop new therapeutic strategies to eradicate relapse-inducing cells, and identify biomarkers for predicting therapy response or relapse in T-ALL and other subtypes of acute leukemia.

